Whipple procedure
The whipple procedure, or pancreaticoduodenectomy, is the most common operation performed to treat pancreatic masses and offers the best chance for long term control of disease.
The procedure is used to treat benign masses or cancers in the head of the pancreas, ampulla of Vater, duodenum, common bile duct and sometimes to treat chronic pancreatitis. The laparoscopic-assisted Whipple is a minimally invasive, complex procedure that requires the skill of highly trained, specialized surgeons to ensure the best outcomes.
Types of procedures
There are two types of whipple procedures done. Your surgeon will discuss with you which procedure is best for you.
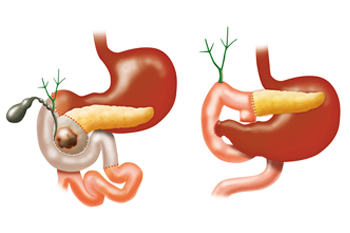
- The modified, or pylorus-preserving (which is most commonly done), does not remove any part of the stomach.
- The standard procedure removes the head of the pancreas, the gall bladder, the common bile duct, the duodenum (the first portion of the small intestine), a small portion of the jejunum (the second portion of the intestine), the pyloric antrum and pylorus (the bottom third of the stomach), and the lymph nodes near the head of the pancreas.
Your surgeon then reconnects the small intestine to the bile duct, remaining pancreas, and stomach.
During surgery
- General anesthesia is given for the procedure. After anesthesia is initiated an ET (endotracheal) tube will be placed into your airway through your mouth and will be attached to a breathing machine (ventilator). The ET tube will assist your breathing while under general anesthesia. An NG (naso-gastric) tube will also be placed through your nose and into your stomach when you are in the operating room to prevent nausea and vomiting.
- Your abdomen will be filled with gas to help your surgeon better visualize your abdominal cavity.
- Three small incisions will be made to perform the procedure. A small camera will be introduced into one of the incision sites (approximately 1/2 inch) to let your surgeon see the pancreas and surrounding area. Your surgeon will inspect the pancreas and surrounding area to ensure that the surgery can still be performed safely. A second incision site of approximately 1/4 of an inch will be used for instruments. The third incision site of approximately 3 1/2 inches will allow your surgeon's hand to guide the operation and remove the involved portion of the pancreas.
- On occasion, upon inspection, your surgeon may decide that the more traditional, open Whipple procedure is necessary to perform and will convert the procedure. Additionally, disease that was too small to be identified on pre-operative scans may be found and would indicate that surgical treatment is no longer appropriate. If the disease has been found to be unresectable, your surgeon will proceed with the necessary steps to minimize any long-term problems that could be caused by the disease.
- The procedure usually takes approximately four to six hours, depending upon each patient and the extent of the disease.
- During surgery, a nurse will come to the surgical waiting area to give updates about the procedure to family and friends. When the procedure is complete, your surgeon will provide a final update.
After surgery
Planning will begin a few days before you are ready to leave the hospital. Your discharge instructions will be given to you the day of discharge. These include:
- Diet: Instructions will be given to you by a nutritionist prior to discharge and will be based on your nutritional intake at the time of discharge.
- Medication: Prescriptions will be given to you before discharge, including medications for pain, medication to help control the secretion of acids created in the stomach and possibly for pancreatic enzyme replacement.
- Pain: Post-surgical pain is common and will improve over time. It is important that you take your pain medication as prescribed. Please let your healthcare provider know if your pain medication is not working (or if it is too strong) so that it can be modified.
- Constipation is common post-operatively due to inactivity and decreased nutrition and fluid intake. It is also a common side effect of the pain medication. A stool softener/laxative should be included with your daily medications.
- Incision care is important. The incision site should be kept clean and dry and will heal over time. The staples used for the surgery will be removed at a post-op visit. A little tenderness and drainage at the incision site is normal, but if you notice increased drainage, a foul odor, increased redness or tenderness, please notify your health care provider.
- Activity after surgery is recommended. You are encouraged to return to all of your normal activities as soon as you feel able, but should not lift anything over five pounds or drive a car until your healthcare provider gives you permission to do so. You may feel some pain as you resume activity; this is normal. A good rule of thumb is to "push to the pain, but not through the pain," If you experience any sharp pain that does not resolve or gets worse, notify your health care provider immediately.
- Follow-up appointments will be given to you at the time of discharge, if not previously arranged, and are usually seven to 14 days after discharge.
- Help at home is available. There are several agencies that can provide support depending upon your specific needs after discharge. Examples of support include skilled nursing, nurses' assistants, physical therapy, nutrition or IV support, and medical equipment. Discuss your concerns and needs with your nurse prior to discharge.
- Recovery time is typically six to eight weeks after surgery and you can plan on resuming normal activities around six weeks post-operatively, but this can vary among patients. Please be patient with yourself, you have just had extensive surgery.
Pathology results
Pathology results are usually ready in approximately seven days after surgery and can be given to you before you leave the hospital if you wish. If not, they will be given to you and discussed at your first post-surgery visit.
Call your healthcare provider
Contact your healthcare provider if you experience:
-
Temperature greater than 100.4 degrees
-
Increased or foul-smelling drainage from your incision site
-
Increased pain or redness at your incision site
-
Pain, nausea, or vomiting that is increased or not controlled by your current medication
-
Diarrhea or constipation that is not controlled
-
Anything that is of concern to you, as only communication with your healthcare team can ensure your best outcome
Learn more about the treatments we offer at MedStar Georgetown Pancreatic Diseases Program:
Our providers

Expert gastroenterology care
Getting the care you need starts with seeing one of our gastroenterologists.









